Things may look alarming to civilians, but Singapore has built upon its experience with infectious diseases to fight COVID-19 in an organized way, including roping in healthcare workers to serve the nation on the screening frontline. City News speaks to healthcare workers who are members of City Harvest Church, two of which are frontline workers at the NCID.

The swift development of the novel coronavirus situation in Singapore, which has the second-largest number of people diagnosed with the virus, has sent the country into a state of alert—but not panic.
If there is one thing Singapore can be proud of, it is that its medical community is well-equipped and situationally-prepared for infectious diseases.
The 1999 Nipah outbreak was the first major infectious disease that caught Singapore off-guard. Profession Leo Yee Sin, Executive Director of the National Centre for Infectious Diseases (NCID) said in a 2014 interview that “The ground was totally unprepared and disconnected [for Nipah]. Cases were drained to CDC (Communicable Diseases Centre), public health aspects such as contact tracing, epidemiology done by then the Quarantine Epidemiology department in Ministry of Environment, food control and operation by Ministry of National Development.”
By the time the SARS epidemic came round in 2003, taking 33 lives in Singapore, “much of the immediate response we put in place for SARS in fact were lessons learned during Nipah outbreak,” Prof Leo said in the same interview. “We were the first to institute triage, one-stop screening clinic, health monitoring of healthcare workers, for example, temperature monitoring.”
Thanks to Prof Leo and the healthcare workers at NCID and Tan Tock Seng Hospital, the way Singapore is handling COVID-19 has become an example for other nations. World Health Organization spokeswoman Olivia Lawe-Davies said, “Before the detection of the first case in Singapore, preparedness activities were already under way for the rapid detection and response to 2019-nCoV, including enhanced surveillance and communication with the public and healthcare workers.”
Although the interview was done six years ago, Prof Leo’s vision for a strong and supportive system has come to pass during this latest outbreak. She said, “Every outbreak tells a story and every outbreak provides new learning points. For every outbreak we’ve been through will enhance and add on to our knowledge and capability. We are as ready as where the current knowledge allows, there will be new things and fresh challenges ahead. It is prudent the system is flexible and responsive. I believe we have come a long way since Nipah and SARS, the system in place will support us through future challenges.”
CHC HEALTHCARE WORKERS ON THE FRONTLINE
Among the 160 frontline healthcare workers manning the 24-hour screening centre at NCID are two Advanced Practice Nurses who are members of City Harvest Church.
Xanthe Chua, 43, and Audrey Wong, 42, volunteered to serve on the frontline when they learned of the urgent need.
“I feel it’s natural to volunteer when you see the hospital’s needs,” Audrey, a psychiatric APN in Tan Tock Seng Hospital (TTSH) explains.
Xanthe is an APN in rheumatology department of TTSH. Seventeen years ago, she also volunteered to do screening during SARS. “I was very junior then,” she recalls. “Mentally it was very different for me—I was more afraid, there seemed to be a lot of unknowns.”
The mother of three explains that she volunteered at the screening center because she knew NCID “really need people. But also because I wasn’t scared—we are more prepared as a hospital. Having gone through SARS, MERS-Cov, Ebola, we know the procedures. Also, being Christians, we are well-protected through prayer.”
Audrey summarizes the screening procedure: “We screen anyone who walks in or comes via referral. We screen them to determine if they are of low or high risk. Then we triage them to determine their physical health status. Every patient gets a chest X-ray. Depending on the doctor’s review, we will do procedures on patients such as taking blood, setting up an intravenous infusion, run an electrocardiogram (ECG), conduct urine tests and swabs to test for COVID-19.”
Most of those that go for screening do not test positive for COVID-19. The ones that are go to the isolation wards, and contact tracing begins.
Xanthe marvels at the timeliness of the NCID building, which was only officially opened in September 2019. The isolation wards were set up for such an emergency.
“Initially screening was at TTSH’s A&E. When more and more people were affected and coming for screening, the hospital decided to open up the screening center with 130 nurses to run it 24 hours a day,” describes Xanthe. “This number barely runs three shifts. The hospital had to source from every department in TTSH. We’re at 160 frontline workers now and we need more people.”
The frontline workers do shift duties: night duty, morning and afternoon duty. They get the day after a night duty to sleep. This is a challenge for APNs like Audrey and Xanthe as their jobs usually have regular hours. “There is some physical adjustment to be made,” explains Xanthe, “because your body clock needs to adjust.”
“It’s intense,” says Audrey. “You see between 100 and 300 persons daily. You work with people you never worked with before. You have to adjust to working shifts. People who come through screening center have different expectations. Some face a language barrier. Some are the worried, and many are sick, coughing away. You have to manage each person differently.”
Xanthe notes that each time there is a new case from a new location, the screening center will swell with numbers coming to be tested.
“Some people walk in demanding to be swabbed,” she says. “But we will look first to see how closely you have been in contact with the confirmed case.”
Though they are in hot zone, neither Xanthe or Audrey entertain fear of bringing the virus home to their families. The personal protective equipment (PPE) worn by frontline staffers are left behind before they go home, and laundered specially for them. Frontline workers go through disinfection procedures when they exit the screening center.
It is an exhausting job, and the situation can be demoralizing. Audrey shares that she holds on to 1 Samuel 30:6, which says “But David strengthened himself in the Lord his God.” “The worship song ‘Way Maker’ also gives me strength,” she adds.
Xanthe admits that there is some discrimination when people see them in their PPE, or when they find out they are healthcare workers. But she draws strength from 1 John 4:4: “You are of God, little children, and have overcome them, because He who is in you is greater than he who is in the world.” She adds, “The prayer that Pastor Kong and Sun prayed for us which was sent to us by WhatsApp is awesome. I play it every day before I start my shift, and pray in agreement.”
On the other hand, there are times they feel the love from the community.
“I think we have received many forms of help and kind gestures,” says Audrey. “One cell group initiated getting coffee for us [with the #BoosterShot movement]. Some sent us sweets and nuts.”
“There are members of the public who would bless us with donuts—one sent 120 donuts to the screening center,” shares Xanthe. “One church pastor came with muffins and cards with encouraging verses—even the non-Christians felt blessed. We also get liang teh (herbal drinks) and one caterer offered to provide lunch for two weeks.”
Part of the PPE are N95 masks and balaclava-style goggles, which are worn tightly to prevent infection. These leave bruises or even broken skin on the face. “Some doctors who are not on the frontline buy us skincare to treat our faces,” says Xanthe. “All these little things make us feel we are not alone.”
BEYOND THE FRONTLINE
It is not just the frontline healthcare workers that are affected by the outbreak. A CHC member who is a doctor working in the A&E department of a hospital shares that at the A&E, he comes into contact with suspected cases often. “But thank God that these cases have all been negative so far.”

The A&E is busier since the onset of COVID-19. “We have seen a surge in the number of people coming in or being referred by polyclinic or private GPs to us for fever and flu cases,” he adds. “We also have to constantly stay updated on the virus’s characteristics and infective process as scientists and clinicians learn more about them. As this plays a huge role in how we identify suspected cases and manage them accordingly.”
Work is physically and mentally exhausting, says this doctor. “In this present time and situation, I think one of the greatest challenge is to stay always vigilant and alert in order to accurately pick up those who are or could be infected with COVID-19, to be on our toes to manage and treat them swiftly, especially when patients conditions acutely deteriorate.”
“I thank God for a strong unity between the healthcare workers, good leadership from the government and cooperation with the general public to work together harmoniously,” he says. “Several new protocols and existing arrangements were able to be adjusted adequately to enable a swift and effective response to try to curb disease spread and provide the right treatment to those who are sick. Ultimately God is still our main hope and as believers, we don’t have to fear for He is with us. He will carry and rescue us, He will sustain us.”
COVID-19’s arrival has meant certain restrictions that affect every hospital worker, not just the ones in the frontline. Radiation therapist, Mabel Lee, explains that across the board at public hospitals, all staff leave has been canceled until at least March 31, including leave that was approved prior to the outbreak. All workers have to have their temperature recorded twice a day, wear masks at all times in all work areas, keep good hygiene, learn processes pertaining to what to do should they suspect a patient might be infected with COVID-19 among other measures.
But it is all for the greater good. Mabel adds, “I feel reassured that the hospital is taking all precautions to ensure that the staff are protected from unnecessary exposure, which also in turn ensures that we are able to give the best care to our patients.”
WHAT TO DO & HOW TO PRAY
The A&E doctor has this advice for the public: “Take care of yourself and look out for your loved ones, especially high risk populations like the elderly and children, or those who have preexisting medical conditions, such as heart or lung conditions—these can be more vulnerable. Do seek medical consultation especially if you have flu symptoms or fever, or f you have had contact with a confirmed patient, or have recently traveled. Avoid crowded places as much as possible and stay hygienic—wash your hands regularly.”

“Clean your hands with soap and water,” Audrey echoes. “Shower. Cover your mouth when coughing. Maintain basic hygiene. And boosting one’s health is good!”
This weekend at service, Pastor Bobby Chaw leads City Harvesters in praying for our healthcare workers and those at the frontline. How would they like us to pray for them?
“Pray for strength to sustain us and wisdom in managing the situation,” says the A&E doctor. “Also it’s important to pray for us to have God’s supernatural protection from the viral infection and all illnesses so that we can remain fit and healthy to continue treating and providing help not just those who are affected by the virus but also the rest of the patients who are in hospital for various other medical conditions.”
“Pray for us to have strength, grace, mercy and compassion,” says Audrey.
Xanthe adds, “Please continue to pray for the frontline people; pray for protection, especially, that none of the medical staff get infected, because that can be scary for the frontline workers. During SARS we lost colleagues. So please pray for our safety and protection.”
Pay tribute to our healthcare workers and those on the frontline by posting your gratitude with the hashtag #sgsalutesyou
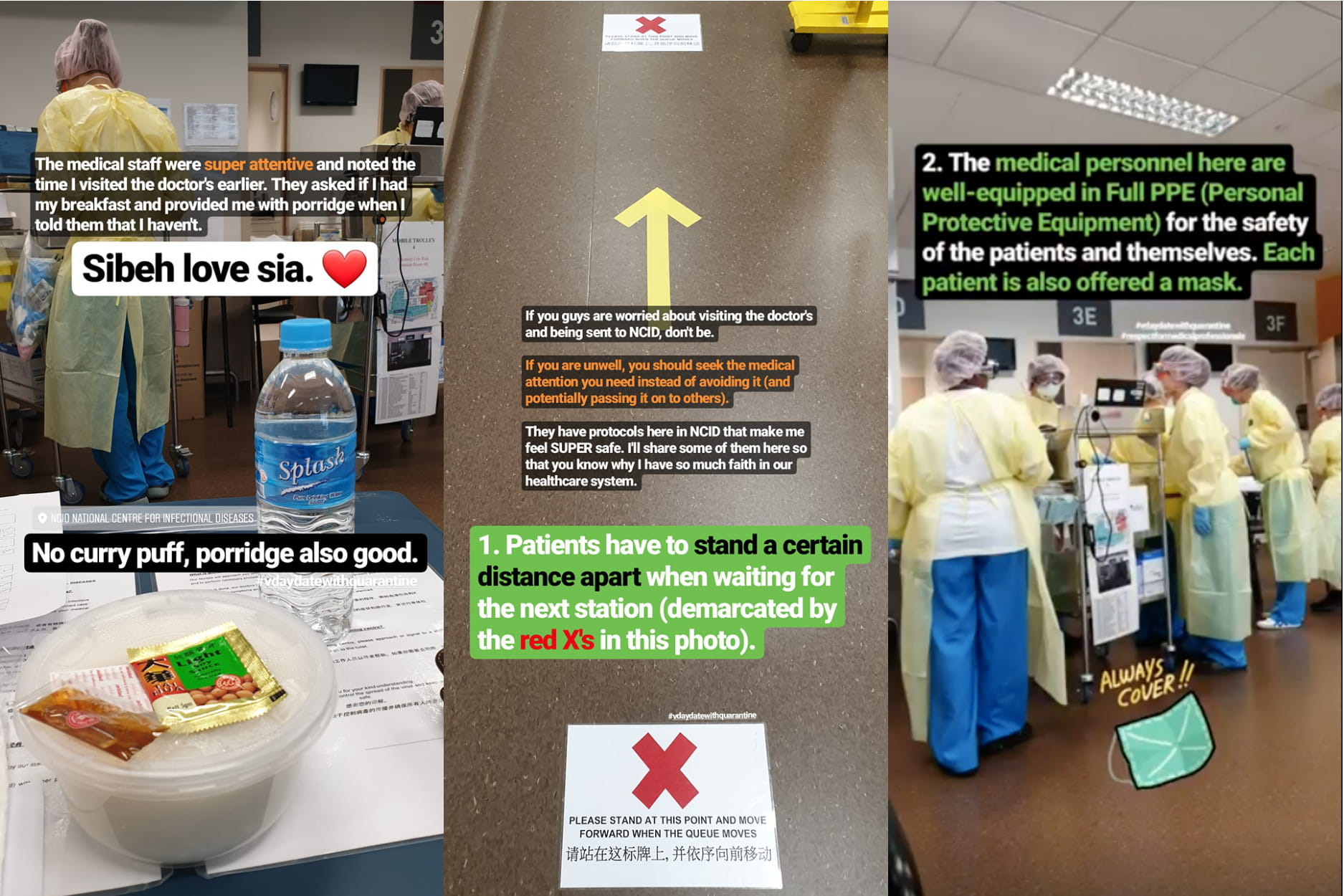
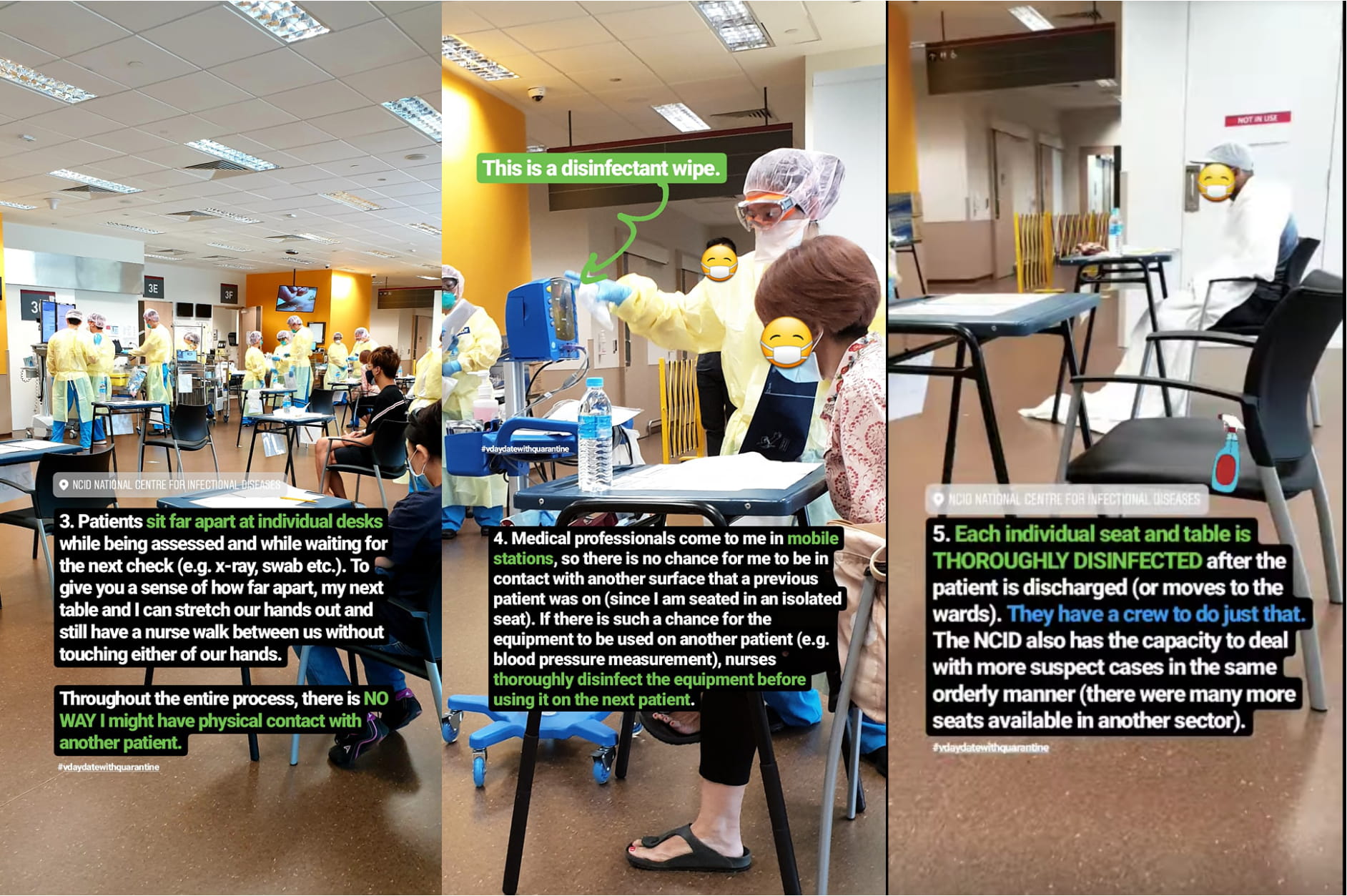
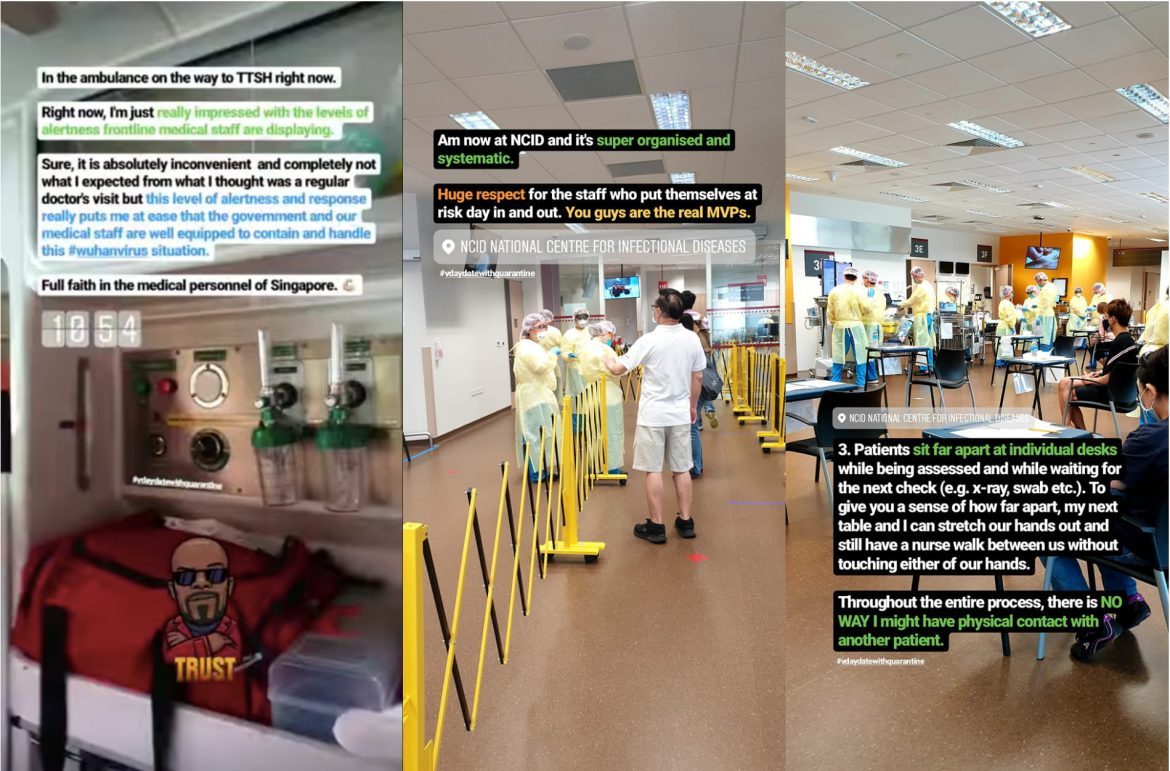
INSIDE THE NCID SCREENING CENTER
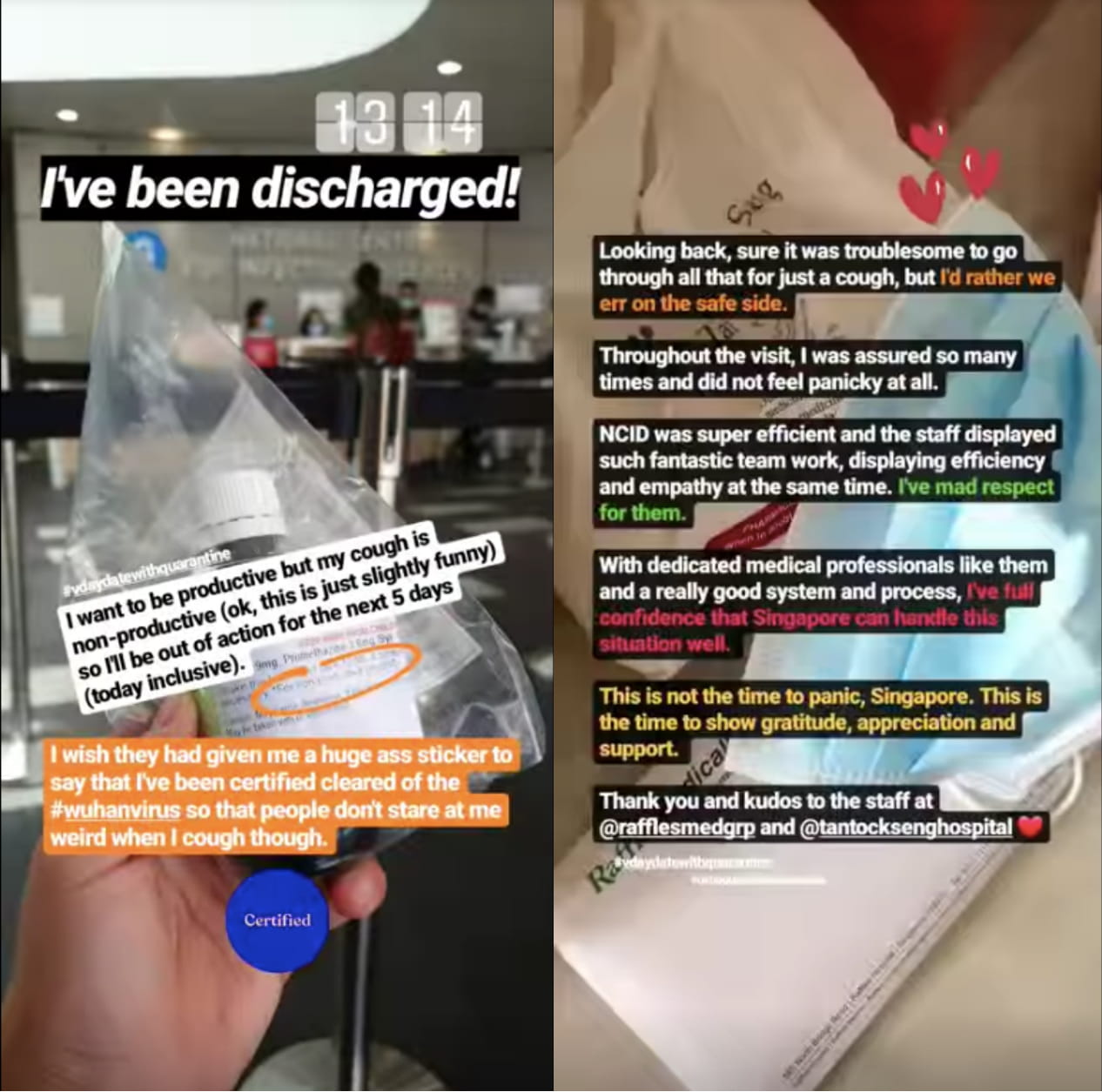
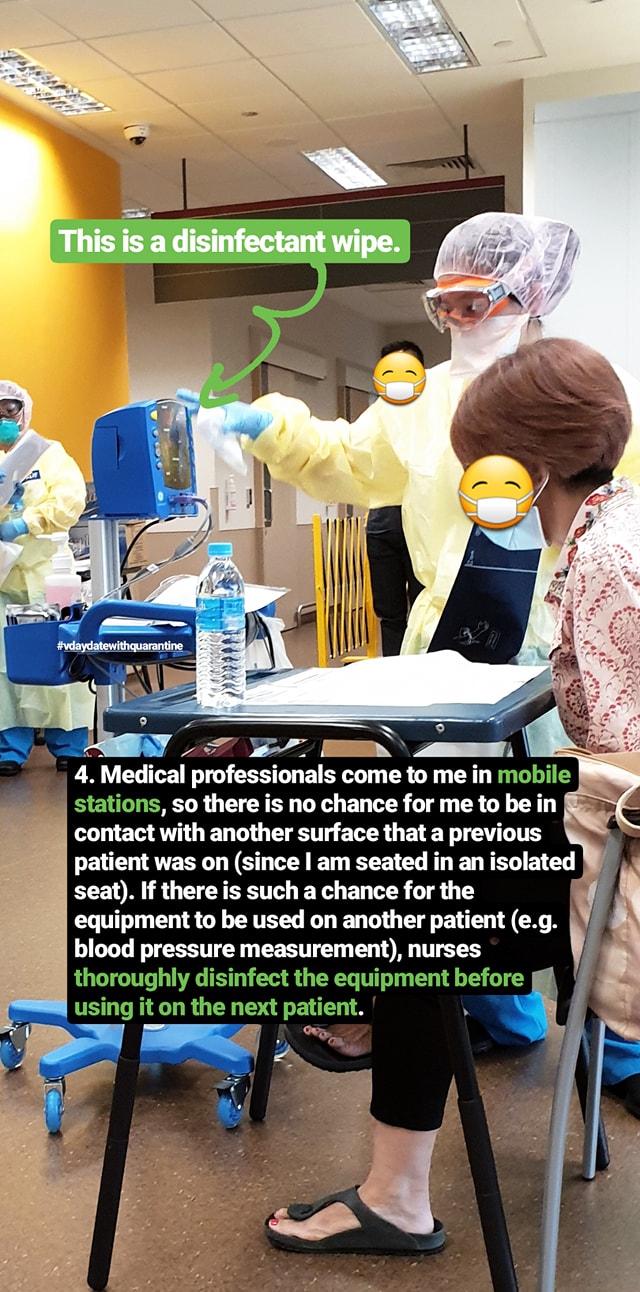
On Feb 14, Facebook user Joyce Chan posted a very interesting and detailed post about undergoing screening at NCID. She had gone to her GP for a cough, but as she had recently returned from Taiwan, she found herself in an ambulance headed for NCID. Her informative yet funny account was shared by many Facebook users.
She took photos of what the inside of the screening center looks like and what the process is.
She wrote:
“Sure, it was troublesome and just slightly alarming that I was sent to NCID but the experience gave me 100% confidence in Singapore’s preparedness to contain and deal with the current #Covid19 situation (or coronavirus / wuhan virus / 2019-nCoV).
“I’ve heard that people are now less willing to seek treatment when they are unwell as they fear being sent to NCID.
“As humans, we often fear what we don’t understand. As such, I decided to document the entire journey in NCID through instastory @joycechansg (from admission, triage, diagnosis to discharge) to help others understand what goes on inside NCID and to give people a greater peace of mind. The medical professionals were efficient and empathetic, and they have a good process and system to ensure that patients have no contact with one another.
“With such dedicated medical professionals and good systems and processes in place, I have full confidence that Singapore can handle this situation well.
“Now, more than ever, is the time to seek treatment if you are feeling unwell (instead of potentially passing any virus on to others).
Kudos to the medical professionals in Tan Tock Seng Hospital (TTSH), Raffles Medical Group and everywhere else in Singapore. You guys are truly the real MVPs and I truly appreciate your hard work during this difficult period.”
Excerpts of post reproduced with permission.